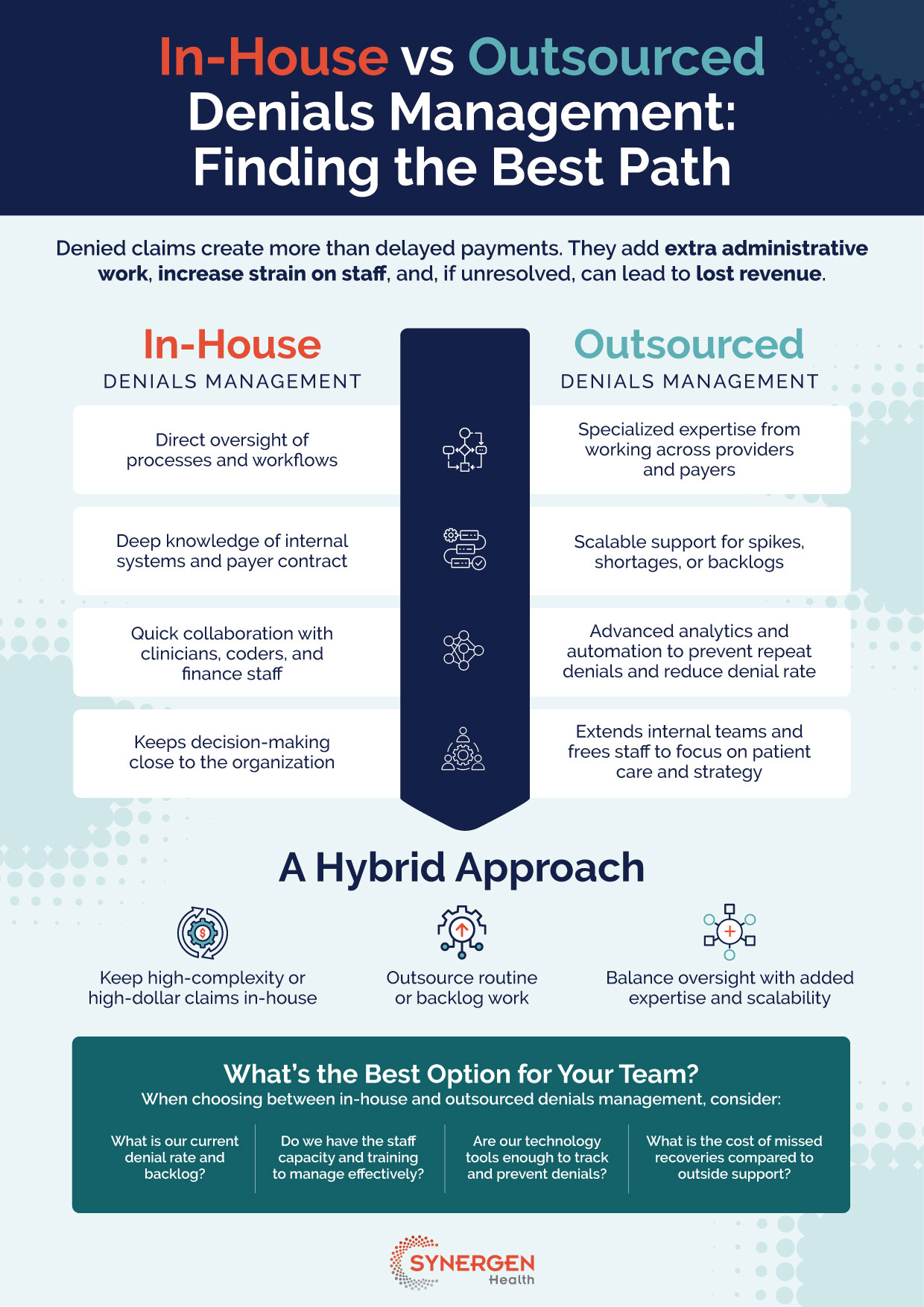
In-House vs Outsourced Denials Management: Finding the Best Path
Denied claims create more than delayed payments. They add extra administrative work, increase strain on staff, and, if unresolved, can lead to lost revenue.
In-House Denials Management
- Direct oversight of processes and workflows
- Deep knowledge of internal systems and payer contracts
- Quick collaboration with clinicians, coders, and finance staff
- Keeps decision-making close to the organization
Outsourced Denials Management
- Specialized expertise from working across providers and payers
- Scalable support for spikes, shortages, or backlogs
- Advanced analytics and automation to prevent repeat denials and reduce denial rate
- Extends internal teams and frees staff to focus on patient care and strategy
A Hybrid Approach
- Keep high-complexity or high-dollar claims in-house
- Outsource routine or backlog work
- Balance oversight with added expertise and scalability
What’s the Best Option for Your Team?
When choosing between in-house and outsourced denials management, consider:
- What is our current denial rate and backlog?
- Do we have the staff capacity and training to manage effectively?
- Are our technology tools enough to track and prevent denials?
- What is the cost of missed recoveries compared to outside support?