2024 marks a pivotal year where technological advancements and operational challenges intersect to shape the future of revenue cycle management.
The industry is at a critical juncture where embracing innovation is not just an option but a necessity to stay competitive and efficient. From the increasing adoption of technology for process automation and the strategic use of data analytics, the current trends in RCM reflect a broader shift towards a more tech-driven, efficient, and patient-centered approach.
Amidst these changes, two key challenges continue to dominate the scene: the increasing complexity of healthcare billing and the persistent issue of staffing shortages and associated rising costs. As healthcare organizations strive to navigate these challenges, technology becomes increasingly central, offering solutions ranging from automating mundane tasks to employing sophisticated AI for strategic decision-making and denial management.
The year 2024 stands as a testament to the transformative power of technology in healthcare RCM, underscoring its potential to streamline operations and enhance patient care, financial sustainability and profitability.
Let’s dive into the top five trends affecting revenue cycles in 2024.
1. Process Automation Evolves from a Trend to a Necessity
Automating portions of the revenue cycle is evolving from a trend to a fundamental requirement in 2024. With patient numbers rising and billing procedures becoming more complex, automating repetitive, manual tasks has never been more critical to a healthy revenue cycle.
In fact, one survey reported that 80% of hospital and health system executives said automation is vital to the success and survival of their organizations.
The right technology can automate activities that span the entire revenue cycle, from patient scheduling and registration to intricate coding and billing. AI-driven systems can manage these tasks with improved efficiency and accuracy, significantly reducing errors and freeing human resources for more strategic roles.
For instance, automated systems in patient scheduling are not just streamlining appointment processes but are also enhancing patient satisfaction by reducing wait times and improving overall service delivery.
In the context of claims processing, automation technology can execute tasks such as verifying patient insurance coverage, checking for coding errors, and submitting claims electronically, which not only accelerates revenue cycles but also minimizes the risk of human errors that could lead to claim denials or payment delays. And with eligibility and missing prior authorization being cited as top reasons for initial payer denials in 2023, the importance of accuracy at these stages is critical.
Moreover, automation is also particularly valuable to the patient side of billing, as AI-powered systems can quickly generate accurate and detailed bills, ensuring an organization can bill patients correctly and promptly. This improves revenue capture and enhances patient experience by providing transparent, error-free billing statements.
2. Leveraging Data Analytics for Increased Visibility During Mergers and Acquisitions
As healthcare organizations grow through acquisitions and mergers, managing their financial operations has become increasingly complex.
In 2024, the importance of having a comprehensive, enterprise-wide view of financial performance cannot be overstated, especially considering that healthcare executives expect M&A activity to continue to grow this year.
The trend of acquisitions and mergers in healthcare underscores the necessity for interoperability and an enterprise-wide view of financial performance. Here, intelligent data analytics powered by AI play a pivotal role.
By leveraging AI and machine learning, healthcare organizations can analyze vast amounts of data to gain insights into operational efficiency, patient flow, and overall financial performance. This level of insight is critical for strategic decision-making, especially in an environment marked by continual growth and expansion.
For example, AI-driven analytics can help a healthcare network identify inefficiencies in patient flow across different facilities, leading to targeted improvements and optimized resource allocation.
Interoperability is another critical aspect of this trend. AI-driven analytics solutions can bridge the gap between disparate systems and data sources, facilitating seamless communication and data sharing between different departments and acquired healthcare groups. This interoperability is key to maintaining a unified and efficient revenue cycle.
EXAMPLE
AI-driven analytics can help a healthcare network identify inefficiencies in patient flow across different facilities, leading to targeted improvements and optimized resource allocation.
3. Transforming Denial Management with AI
Denial management remains one of the most challenging aspects of RCM. And with denials on the rise—Medicare Advantage denials went up by 56%, and commercial denials jumped 20% in 2023—AI’s role in tackling this challenge is becoming increasingly significant in 2024.
With the help of AI, we can now move from denial trending to predictive denials and prescriptive changes, leading to one-touch denial correction.
Imagine a scenario where an AI system can quickly pinpoint common reasons for claim denials, such as coding errors or missing documentation. With this insight, healthcare organizations can proactively address these issues, improving their overall claims acceptance rate and reducing the time and effort spent on future denial management.
If an organization still receives a denial, AI-powered workflow management tools can pull from historical data to map the most appropriate responses that previously resulted in one-touch fixes.
For example, say a denial comes back requesting additional detailed information; our AI-driven denial management system starts an automated appeal process where it retrieves relevant data, such as operation notes, and refiles the claim with the necessary documentation. Or, if a payer seeks more precise details, such as the number of medicine units given to a patient, it can pull this information from the operation notes and prepare the claim for resubmission.
Closing the loop, AI-powered tech can also learn and adapt to changing reimbursement rules and regulations, ensuring healthcare organizations stay up-to-date and compliant with payers.
EXAMPLE
If a denial comes back requesting additional detailed information; our AI-driven denial management system starts an automated appeal process where it retrieves relevant data, such as operation notes, and refiles the claim with the necessary documentation.
Or, if a payer seeks more precise details, such as the number of medicine units given to a patient, it can pull this information from the operation notes and prepare the claim for resubmission.
4. Increase in Outpatient Procedures in ASCs
2024 brings a notable surge in outpatient procedures conducted in ambulatory surgery centers (ASCs), primarily due to the expanded approval of various procedures traditionally reserved for hospitals.
This transition is driven by a growing recognition of the efficiency, cost-effectiveness, and patient convenience offered by ASCs. Procedures such as advanced endoscopies, certain orthopedic surgeries, and minimally invasive operations, which once necessitated hospital admission, are now routinely and safely conducted in ASCs.
The shift from a hospital setting to ASCs for outpatient procedures can significantly impact the revenue cycle within these centers. For ASCs, the increase in the variety and volume of procedures presents an opportunity for substantial revenue growth.
However, it also brings about challenges in terms of billing and coding complexities. Unlike hospitals, ASCs often operate with more streamlined administrative processes and may lack the extensive infrastructure to handle the intricacies associated with a broader range of procedures.
This necessitates adapting their revenue cycle management, potentially requiring upgraded billing systems, enhanced coding expertise, and refined patient billing practices to ensure accurate reimbursement and compliance with healthcare regulations.
Potential RCM changes for ASCs to ensure accurate reimbursement and compliance with healthcare regulations:
- upgraded billing systems
- enhanced coding expertise
- refined patient billing practices
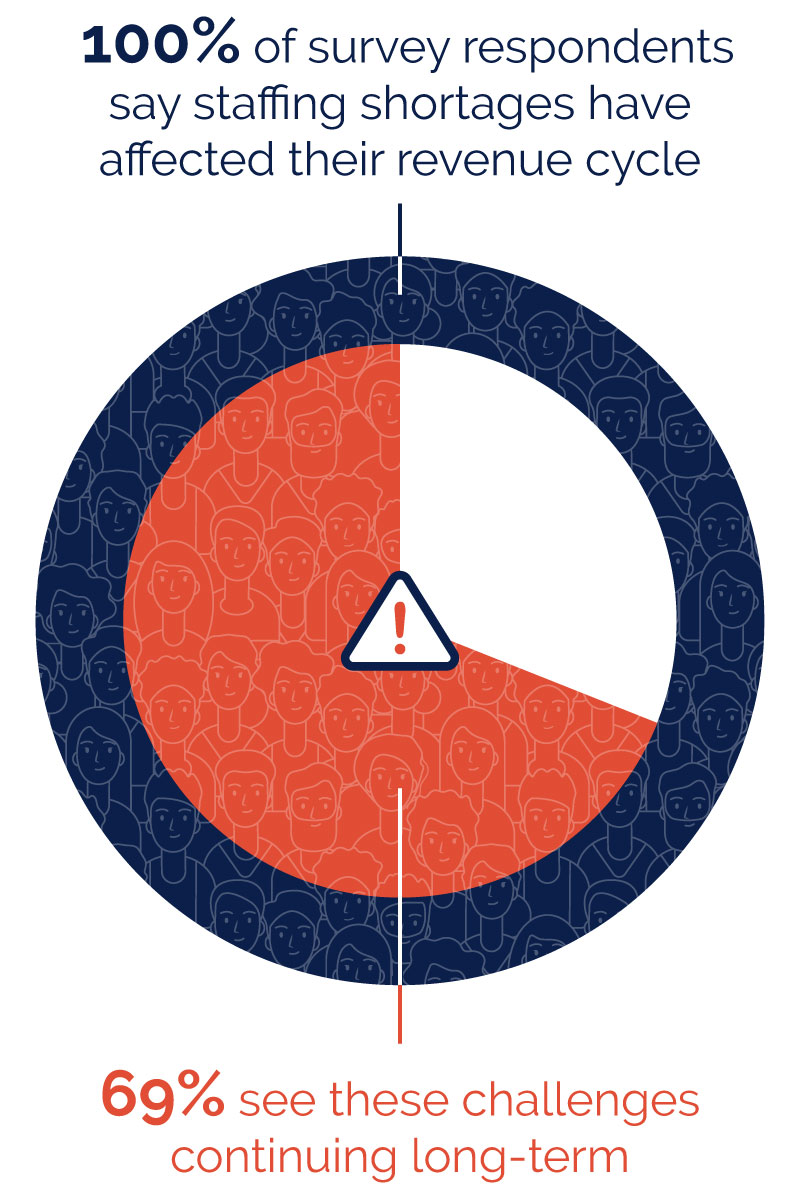
5. Staffing Challenges Will Persist
While technology is advancing rapidly in healthcare RCM, staffing challenges are expected to persist in 2024 as the demand for skilled RCM professionals continues to outpace the supply.
According to one survey, 100% of survey respondents say staffing shortages have affected their revenue cycle and 69% see these challenges continuing long-term.
To address this challenge, healthcare organizations may need to invest more in training and development, explore innovative staffing models, and leverage technology to streamline RCM processes.
Additionally, AI-driven RCM solutions can complement the workforce by handling routine tasks, freeing staff to focus on more complex and value-added activities.
Embracing Advanced RCM Solutions for Success in 2024
It’s evident that the healthcare industry is set on a path where continuous innovation and adaptation will be key to success. Integrating technology into RCM is not just about keeping pace with change but about leading and shaping the future of healthcare delivery.
Finding the right end-to-end RCM service partner, or a partner that offers specific point solutions, is essential for healthcare organizations looking to navigate the complexities of today’s healthcare landscape effectively.
Our team of RCM experts is ready to help your organization identify and implement the ideal RCM solutions tailored to meet your specific needs and challenges.
Let us create a customized RCM roadmap for your organization so you can usher in a new era of profitability and innovation in 2024.